Are you going Through Menopause? You may be experiencing Vaginal Atrophy
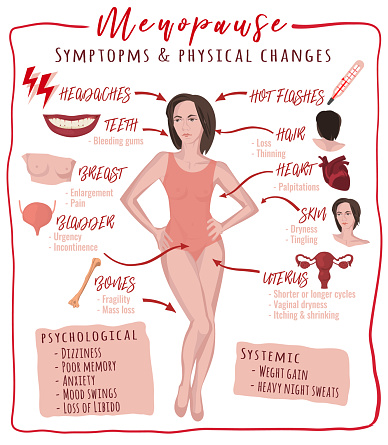
Are you going through menopause? As women age, our bodies go through many changes. It feels like a second puberty with menopause and everything that comes with it. It can be a challenge trying to know what to expect. In today’s article, we will be going over one of the conditions you may experience during menopause, how to spot it, and what you can do for treatment.
What is it?
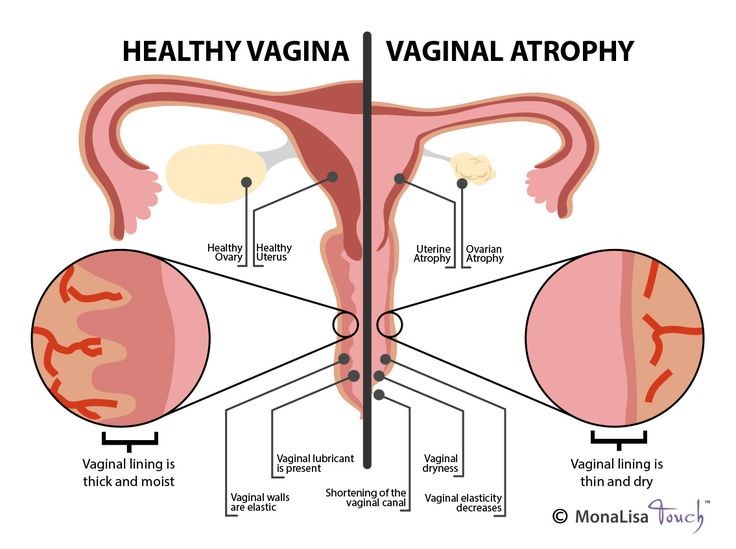
Vaginal atrophy (atrophic vaginitis) is thinning, drying and inflammation of the vaginal walls that can arise when your body has less estrogen. Vaginal atrophy occurs most frequently after menopause, or pre-menopause. For many women, vaginal atrophy not only makes
intercourse more uncomfortable, but also leads to distressful urinary symptoms. Because the situation causes both vaginal and urinary symptoms, doctors use the term “genitourinary syndrome of menopause (GSM)” to describe vaginal atrophy and its additional symptoms. Reduced estrogen levels result in changes to your body, but it doesn’t mean you have to live with the worrying symptoms of GSM.
What are some of the symptoms?
Usually, a healthcare provider can diagnose vaginal atrophy based on your symptoms and a pelvic exam to look at your vagina and cervix. Classic signs of atrophy during a pelvic exam include: A shortened or narrowed vagina, Dryness, redness and swelling, Loss of stretchiness, whitish discoloration to your vagina, Vulvar skin conditions, vulvar lesions and/or vulvar patch redness, Minor cuts (lacerations) near your vaginal opening, & decrease in size of the labia.
What can cause it?
Women in menopause/pre-menopause are at a higher risk for vaginal atrophy, because their body is creating less estrogen. There are also other causes and situations that lead to vaginal atrophy as well, including the following: Decreased ovarian functioning due to chemotherapy or radiation therapy, Medications that contain antiestrogen properties including tamoxifen, medroxyprogesterone and nafarelin, Oophorectomy (removal of your ovaries), Some birth control pills, Immune disorders, Breastfeeding (chest feeding), Smoking cigarettes, etc.
While healthcare providers typically rely on examinations to diagnose atrophic changes or GSM, they may do the following tests to rule out other conditions: Pap test, Urine sample, Ultrasound, Vaginal pH (acid test),Vaginal infection testing.
What can I do to prevent or lessen symptoms?
Have no fear, there are many ways to treat this condition! One of the things that can help with reducing symptoms/helps prevent this condition is sexual activity. Activity, with or without a partner, can lead to more mild cases later in life. This is because sex/sexual stimulation increases blood flow to the vagina, allowing the vaginal tissue to be more elastic. There is also vaginal estrogen, which has the benefit of
being efficient at lower doses and reducing your overall exposure to estrogen, because less reaches your bloodstream. It may also provide better direct relief of symptoms than oral estrogen does. Vaginal estrogen therapy comes in a number of forms. Because they all seem to work equally well, you and your doctor can decide which one is best for you. There are also additional treatments if the lack of estrogen comes from cancer/cancer treatments. In consultation with your cancer specialist (oncologist), your doctor might recommend low-dose vaginal estrogen if nonhormonal treatments don’t help your symptoms. However, there’s some concern that vaginal estrogen might increase your risk of the cancer coming back, especially if your breast cancer was hormonally sensitive. Systemic estrogen treatment generally isn’t recommended, especially if your breast cancer was hormonally sensitive.
While these are a few potential treatment plans; we recommend speaking to your OB/GYN or your doctor to find the solution that works best for you and your body.



Leave A Comment
You must be logged in to post a comment.